NHS England has published a new Clinical Waste Strategy which will drive a 30% reduction in carbon emissions and help the health service to meet its net-zero targets.
The document aims to improve waste management practices among NHS trusts, NHS foundation trusts, and primary care operators to make them more efficient and sustainable in order to save on cost, improve function, and reduce the impact on the environment.
The rolling 10-year strategy focuses on improvement in six key areas: data, workforce, compliance, commercial, infrastructure and sustainability.
And it is estimated that it will save the NHS up to £11m every year in recurrent revenue costs while also saving 29,540 tonnes a year of whole-life CO2e – around 30% of the CO2 from this area and equivalent to an estimated two million road miles a year.
In his foreword, Simon Corben, director of estates and head of profession at NHS England, says: “Every year, NHS providers produce approximately 156,000 tonnes of clinical waste that is either sent to high-temperature incineration (HTI) or for alternative treatment (AT), which is equivalent to over 400 loaded jumbo jets of waste.
As one of the largest producers of waste in the country, it is vital that the NHS disposes it in a safe, efficient, and sustainable manner, and we are only creating waste when absolutely necessary
“This has a significant environmental impact and is associated with high running costs and carbon emissions.
“Therefore, as one of the largest producers of waste in the country, it is vital that the NHS disposes it in a safe, efficient, and sustainable manner, and we are only creating waste when absolutely necessary.
“This clinical waste strategy has been created to support NHS providers in making the necessary step change in waste management practices.”
A chronological timeline of the NHS Clinical Waste Strategy measures of success and their target dates, spanning from 2023-2030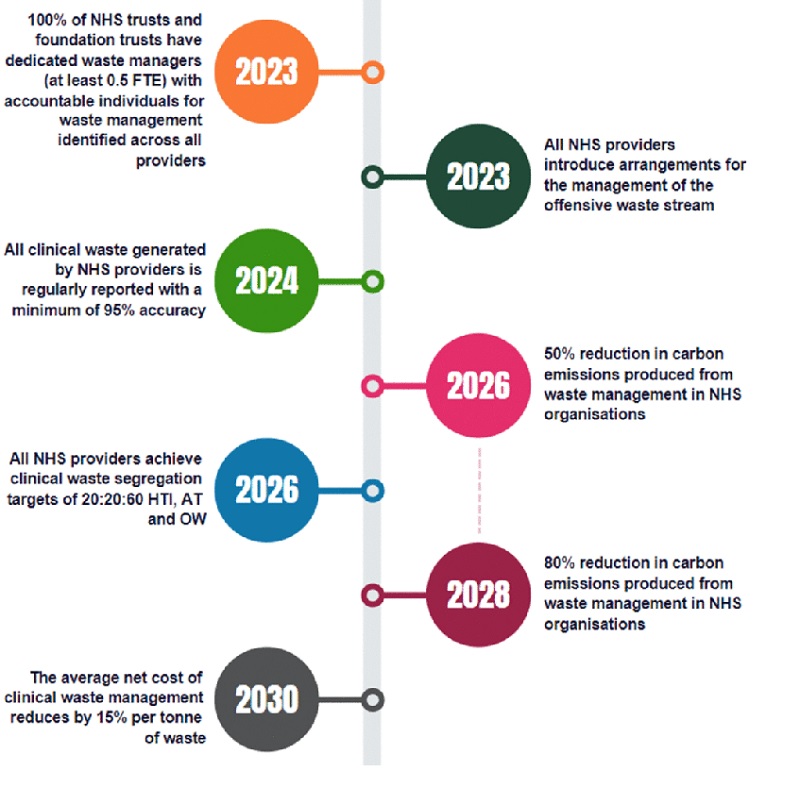
The strategy is part of a suite of documents including the HTM 07-01 and the NHS Waste Planning Tool which have developed to set the direction, trajectory, and speed of change necessary to reach the NHS target of net zero for direct carbon emissions by 2040, and net zero for indirect carbon emissions by 2045, and to ensure the NHS is using its resources effectively.
Corben said: “The best waste management practices reduce waste, improve compliance, and can lead to significant cost savings from lower waste volumes. They also have a significant part to play in minimising harm to the environment and increasing resource utilisation.
“This all leads to a reduction in carbon generated from waste and saving taxpayers’ money.
The best waste management practices reduce waste, improve compliance, and can lead to significant cost savings from lower waste volumes
“This strategy also encourages the use of innovation to increase NHS waste management resilience, improved data use to help guide decision making, and improved staff engagement and training to improve compliance and seek out carbon reduction opportunities in the system.
“In our journey to reduce waste to an absolute minimum, there will be many opportunities to review the materials we use and to find ways of re-using, remanufacturing, or recycling, thus turning them into valuable resources for future use.
“I encourage all NHS providers to embrace and adopt this strategy and embed the steps from the action plan as part of their daily waste management practices.”
The publication of the strategy has been widely welcomed.
Speaking to BBH, Donald Macphail, chief operating officer for treatment at waste management specialist, Veolia UK, said: “The new strategy will enable healthcare to advance the management of complex waste streams.
“By using the latest technologies across data collection and monitoring, waste segregation, and treatment, companies like Veolia can help the NHS to benefit from increased sustainability and lower costs while maintaining essential compliance and safety.
“From our operations, which serve over 200 healthcare facilities, we know that innovation and infrastructure, backed by training, is key to implementing this strategy and these new processes are already set to exceed the target of 50% carbon reduction by 2026.”
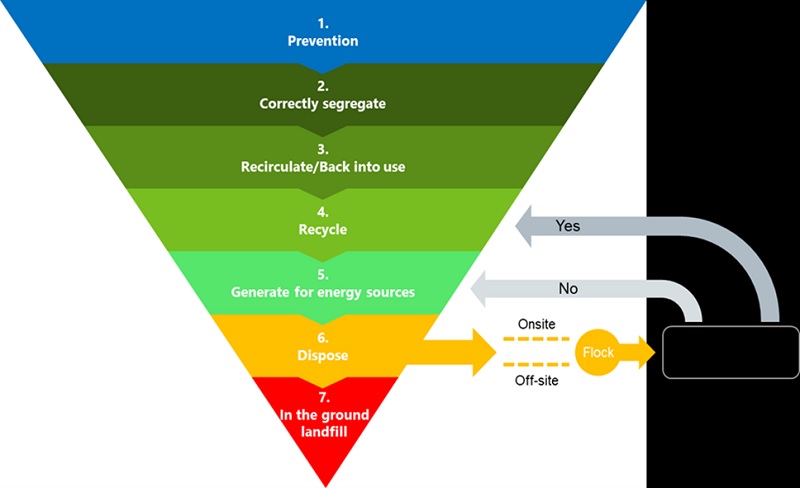
There are seven levels to the waste hierarchy, signifying the most to the least-desirable clinical waste management techniques from an environmental perspective, beginning with the least harmful at Level 1
The six focus areas
- 1. Data: Utilise comprehensive, consistent data from across all NHS organisations/ICSs to drive decision-making and pro-active risk management so that all clinical waste generated by NHS providers is regularly reported, with a minimum of 95% accuracy by 2024
- 2. Workforce: Invest in developing a skilled and diverse waste management workforce with appropriate support and defined career paths, with 100% of NHS trusts and foundation trusts having a dedicated waste manager by 2023, funded from their own resources, and 100% of other NHS providers having identified accountable individuals for waste management
- 3. Compliance: Ensure all NHS staff understand and adhere to compliance requirements so that NHS providers achieve clinical waste segregation targets of 20:20:60 High temperature incineration (HTI), Alternative Treatment (AT), and offensive waste (OW) by 2026
- 4. Commercial: Support the standardisation of contracting arrangement and develop a commercial model which encourages health market conditions so that the average net cost of clinical waste management reduces by 15% per tonne of waste by 2030
- 5. Infrastructure: Invest in clinical waste infrastructure to increase capacity and regional resilience and support sustainable waste processing practices, with all NHS providers introducing arrangements for the management of the offensive waste stream by 2023
- 6. Sustainability: Pro-actively work to reduce harmful emissions, improve local air quality, and achieve the 2045 net-zero carbon target to achieve a 50% reduction in the carbon emissions produced from waste management by 2026, and an 80% reduction by 2028-32




