Despite the COVID-19 pandemic significantly increasing the adoption of technology across the NHS, healthcare professionals are still spending more than 13 hours a week creating clinical documentation, according to a recent report.
But this time, and the associated costs, could be dramatically reduced if electronic patient record (EPR) systems were underpinned by speech recognition solutions, it has been claimed.
The report, from conversational AI pioneer and Microsoft company, Nuance, and independent research consultancy, Ignetica, revealed healthcare professionals were spending an average of 13.5 hours a week adding to, or creating, clinical documentation – more than a third of the average clinician’s working hours and a 25% increase over the last seven years.
Based on an extensive survey of 966 NHS healthcare professionals from four acute trusts and one mental health and community trust; the research gleaned insights around the burden doctors, nurses, and allied health professionals face in their day-to-day roles when it comes to producing accurate and timely clinical documentation.
And it followed a 2015 report, showing that, although much has happened in healthcare over the last seven years, many of the documentation challenges clinicians face have remained the same, or worsened.
Despite the many technological advancements that have taken place in healthcare over the last seven years, the burden of clinical documentation remains
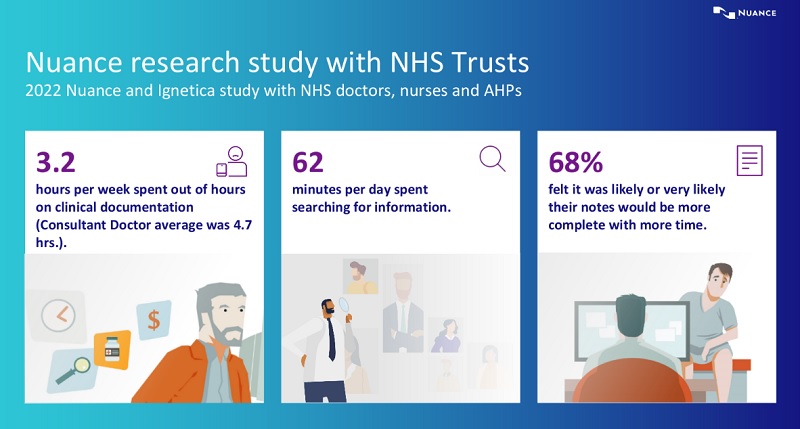
In fact, the report found that the value of time for a consultant doctor searching for missing information and generating clinical documentation is around £57,000 per doctor, per year.
The problem is particularly impacting consultant nurses/nurse practioners (16.5 hours) and non-consultant doctors (15.1 hours).
It is also impacting on the recruitment and retention of staff as the research revealed that healthcare professionals spend an average of 3.16 hours a week adding to clinical documentation in their personal time – with consultant doctors reporting an average of 4.72 hours.
The time spent adding to documentation has increased significantly in the past seven years, despite widespread adoption of electronic patient record systems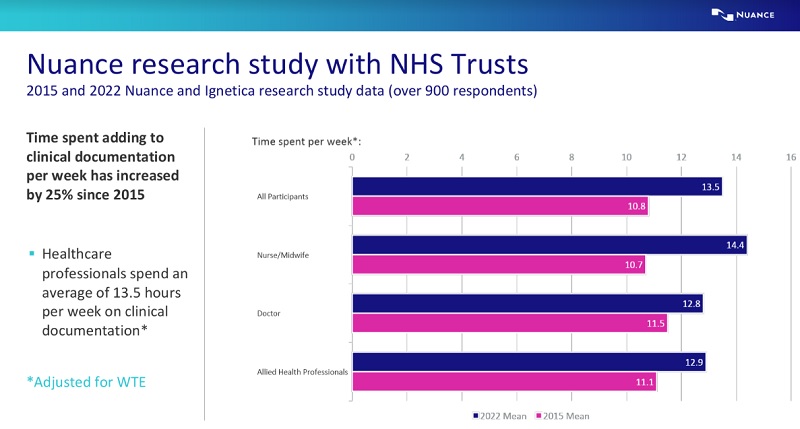
Dr Simon Wallace, chief clinical information officer at Nuance, said of the findings: “Despite the many technological advancements that have taken place in healthcare over the last seven years, the burden of clinical documentation remains.
“As workloads continue to grow, and healthcare organisations are forced to operate with more-limited resources, we are at risk of placing one of our most-precious institutions under even more avoidable pressure.
“And, if nothing changes, we are likely to see many healthcare staff suffering from burnout, which can have serious repercussions for the entire population.”
Less than half (40%) of respondents cited pen and paper as a main documentation format – a positive development since the 2015 study, when 80-90% of clinicians relied on this modality.
Dr Wallace said: “As more clinicians shift to using the EPR to complete their documentation, notes are becoming more structured.”
If nothing changes, we are likely to see many healthcare staff suffering from burnout, which can have serious repercussions for the entire population
However, despite the switch from pen and paper to digital platforms like EPRs, there has not been a significant increase in documentation availability and accuracy.
In fact, in a quarter of instances, clinicians report the information they need is not available in the records at the right time.
The number one cause for this is unclear and incomplete information in the clinical notes or records (36%). Clinicians also report a significant increase in time waiting for diagnostics and investigation results (23%) and, in some instances, uncertainty as to what diagnostics have been requested (19%).
“These challenges add to the time clinicians need to spend wrestling with documentation throughout the day,” said Dr Wallace.
“In fact, despite an increase in digitisation, clinicians are still spending an hour a day looking for missing information and every hour a clinician spends on creating, or locating, clinical documentation is one less hour spent on patient care.
“To enable them to get back to doing what they trained for, we must find new ways to help ease the growing burden of administrative responsibilities.”
And these ‘new ways’ lie in proven and readily-available technology, which can be used to improve the way EPRs work for healthcare professionals.
To enable them to get back to doing what they trained for, we must find new ways to help ease the growing burden of administrative responsibilities
“When I saw the results, I realised the importance of technology such as speech recognition in helping clinicians to access and complete documentation and to encourage the adoption of, and better use of, EPRs,” Dr Wallace said.
“Being able to use automatic text creation and voice control to navigate around the EPR saves time and the associated costs.
“If we can give them the tools that take them to the information they need just by using their voice, then we can take away a lot of the burden.”
However, many trusts opt to introduce speech recognition solutions at the same time, or after, rolling out an EPR.
And, argues Dr Wallace, this is too late!
“Where we have found the technology works best is where trusts roll out speech recognition to all clinicians six, nine, or 12 months before the EPR ‘go live’ so they can get used to it.
“Because speech engines are cloud based and work ‘straight out of the box’, they are fast and accurate and accessible anywhere in the hospital or healthcare organisation, in the office, at home, or even when travelling.
“And, once they embrace this shift away from a keyboard and experience the benefits, the EPR rollout is much easier.
My advice to trusts is to embrace this technology as soon as possible as a tool for enabling EPRs to work more effectively
“My advice to trusts is to embrace this technology as soon as possible as a tool for enabling EPRs to work more effectively.
“It’s not the answer to everything, but it will chip away at the problem, giving healthcare professionals the information they need without the added pressures.
“If more trusts look to procure speech recognition and smart tools within the EPR then it will reduce some of the problems highlighted in this report.”
Doctors feel that with more time they would be able to cafrry out their jobs more efficiently
The benefits of speech recognition
Nuance’s Dragon Medical One is a secure, cloud‑based speech platform for doctors, nurses, and allied health professionals to securely document complete patient care in the EPR, anytime, anywhere.
The solution is 3‑5 times faster than typing, and the speech‑to‑text function feeds directly into the EPR, helping to eliminate errors and delays caused by indecipherable handwriting or poor‑quality audio recordings.
This makes it easier for clinicians to record more-detailed and accurate notes, providing clinical coders with richer detail upon which to determine the coding and reducing the need to seek clarification from clinicians.
Integrating speech capabilities into clinical processes speeds the return on an EPR investment and improves clinician satisfaction and their productivity by at least 10%‑15% per day.
In addition, Dragon Medical One requires no voice profile training.
With a cloud-based user profile, the clinician can use this anywhere in the hospital, in different hospitals, as well as from home.
The speech engine is powered by smart AI algorithms and deep learning and combined with a medical dictionary, the accuracy and word recognition is extremely high.
And the speech engine in Dragon Medical One is very good at recognising different English accents, thus providing even greater accuracy and an optimal clinician experience.
