Like many trusts, Wye Valley NHS Trust (WVT) relied on paper-based prescribing processes, which was based on an original model first created in the 1960s.
This involved extensive use of handwritten drug charts and requisitions, which were delivered to pharmacies by hand, air tube, or, in the case of the three community hospitals, by fax.
The trust has approximately 500 medical and 100 non-medical prescribers handwriting prescriptions for inpatients and outpatients across all sites, which includes three community hospitals.
Recognising the very-serious risks associated with this approach, such as illegibility, lost charts, and prescription and transcription errors which can result in serious and potentially-fatal outcomes for patients; EPMA was made a priority within WVT’s wider digital strategy.
After a competitive tender, in which the various systems were also trialled by the end users, Better Meds scored best in terms of the functionality that the trust was looking for and received the best score from staff demos in terms of usability, while being comparable on costs.
However, before the implementation project had really got going, we had to pause the project due to the COVID-19 pandemic.
The secret is to plan for the unexpected, be adaptable, but stick to your goals and reach out to the influencers and networkers
Despite this, when we were eventually able to reinstate work, we managed to go live on our pilot ward in October 2020, just six months after the system was first accessible to the trust.
And, by December, Better Meds was live across eight wards and within nine months we had rolled it out across 95% of the trust’s sites, including the three community hospitals.
So, how did we achieve such a fast and effective EPMA rollout?
The secret is to plan for the unexpected, be adaptable, but stick to your goals and reach out to the influencers and networkers.
Plan for the unexpected
When we began planning our EPMA rollout, we could never have foreseen that a global pandemic would hit and stop all non-essential work – including implementation of new IT systems.
But that wasn’t the only challenge.
There were many – a new hospital building opened, wards merged increasing bed capacity by 50%, and we were unable to launch on a ward as planned.
All this had the potential to derail our go-live targets and cause costly delays – something that we could ill afford when dealing with medicine management and prescribing.
Fortunately, though, we didn’t have just one go-live scenario and were prepared to adapt.
For example, when we wanted to start the rollout another IT project was supposed to go live. That meant that we couldn’t take nurses off the ward for an hour for EPMA training.
We agreed as a team to delay our rollout by two weeks.
In our sector, people are very willing to help and offer advice – and this proved invaluable
Initially, the two pilot areas were intended to take three weeks each. But, after this unplanned delay, we shortened these to keep on schedule and ensure the delays wouldn’t impact other planned rollouts.
The lesson here: always be aware of what else is going on in the hospital and the wards you’re aiming to work in.
In the end, we had seven go-live scenarios due to the various challenges that we faced along the way.
Build your network
When I joined the EPMA project at Wye Valley, I had already worked at five trusts and implemented several different systems. As a result, I had a ready-made network of colleagues that I could go to for advice.
I also reached out to Taunton and Somerset NHS Foundation Trust and University Hospitals Plymouth NHS Trust who were both implementing Better systems.
In our sector, people are very willing to help and offer advice – and this proved invaluable.
As with all digital transformation, resistance to change can be an issue. So, how do you smooth the way?
Involve the end users – your doctors, nurses, pharmacists and anaesthetists – from the start.
Ask them questions and address their concerns and you will create an atmosphere of ownership and partnership.
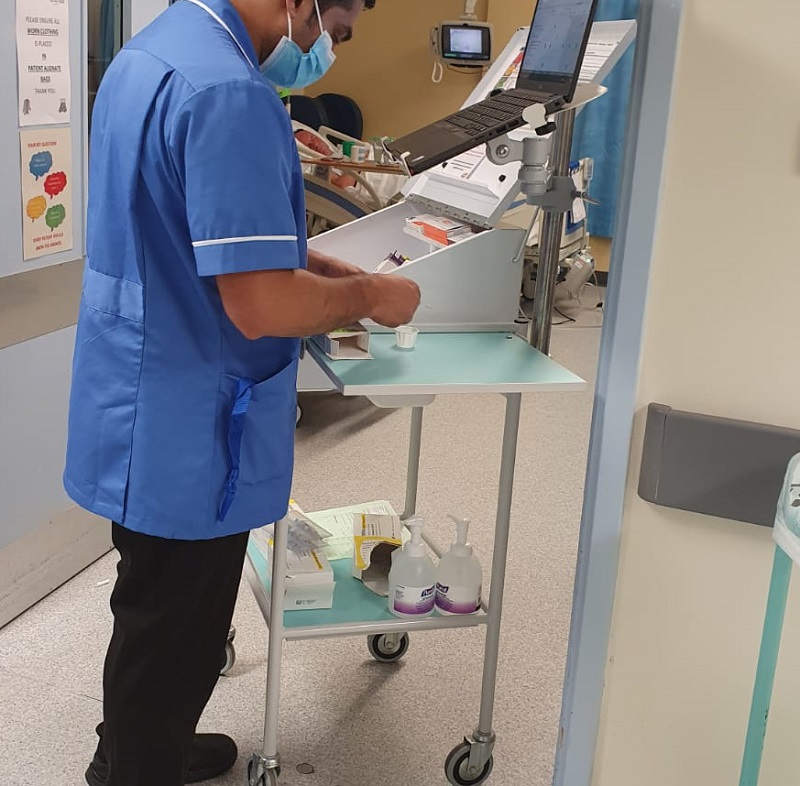
We knocked on doors, joined ward rounds, and gave end-users a laptop so they could play around with the system.
We also organised a roadshow - a stand in the canteen with chocolates, green and black pens, and posters about EPMA Myth Busters where people could ask us anything.
Just as important is top-level buy-in.
Two of the most-crucial aspects of achieving implementation at pace is sticking to your deadline and being realistic
At Wye Valley, the project board had already been created before I joined the team.
However, I lucked in – it’s probably one of the best project boards I’ve ever worked with.
We had the clinical director of pharmacy, the financial director, the medical director, and the nursing director all on the project board.
Even if the board level was unable to help us, the individuals on the board were the ones who could take those issues up to the next level – the executive board.
The solution was live across 95% of the trust's sites within just nine months
Be realistic and stick to deadlines
Two of the most-crucial aspects of achieving implementation at pace is sticking to your deadline and being realistic.
While it is ill-advised to be inflexible when leading a project, the one aspect that I am not flexible on is the go-live deadline because project delays can lead to safety concerns if you end up operating with some wards on paper and some digital.
So, once you have decided on your deadline, you will need to manage the expectations with your end users as to what your EPMA will do.
At Wye Valley, we didn’t go live with VTE assessment, for example; as we didn’t have full integration with laboratory systems.
Yes, that would have been brilliant, but a paper chart doesn’t have those functionalities either.
The EPMA was already much better than the original piece of paper we had been using.
Incentivise engagement
Another challenge resulting from the pandemic was that in-person training was suddenly not an option and the increased workload meant that staff had even less time to engage.
We had to move training online, which while it gave staff the autonomy and flexibility to learn about the system at a time convenient to them, it also ran the risk that they wouldn’t complete the training ahead of implementation on their wards.
We tackled this by incentivising engagement by getting the nurse training course accredited with the Royal College of Nursing.
This gave nurses a nudge to complete the training, even from home, as they knew they would have a certificate for revalidation.
Be present and available
During rollout, we made sure that, as an implementation team, we were on hand to assist with any additional training or troubleshooting. We were available from 7am-10.30pm – as these were the core hours that the wards needed our support.
While it is ill-advised to be inflexible when leading a project, the one aspect that I am not flexible on is the go-live deadline because project delays can lead to safety concerns if you end up operating with some wards on paper and some digital
We were then available outside these hours through an on-call system.
This made sure our staff felt supported and reassured that they would have the help when they needed it.
We also put steps in place so that staff on wards that had already gone live could support those wards that followed, particularly if requests were clinical.
We ensured that we learnt from any issues that did arise and adapted our training so that on subsequent rollouts, we received fewer support calls.
To be available 24/7 is tiring, but the trust welcomed the support, could see how hard each of us worked individually to support them in a time of change, and this, in turn, gave them confidence in us, the system, and the ability to proceed.
Find success
Ultimately, we wouldn’t have been successful in our implementation if we were discouraged by the challenges that came our way.
We all work in clinical environments, and unexpected events do happen. So, when they arrive, don’t just put your blinders up. Use your team and the skills that you’ve learned from going to site visits – from having a clear target and stakeholder management and having a good team structure.
Look for a workaround to any issues that arise and reach out to your network for advice and whether they have encountered similar challenges.
It may require more work, but the satisfaction is so much higher when you hit the targets in the end.
