There has never been a more topical time to talk about the future of independent healthcare estates in the UK.
The balance between the roles of the private and public sectors is thin tightrope. Bringing experts with decades in the sector together to talk about this balance can shine a light on how healthcare construction professionals view this debate.
We should focus on high-volume low-complexity work
The answer, like always, is not simple.
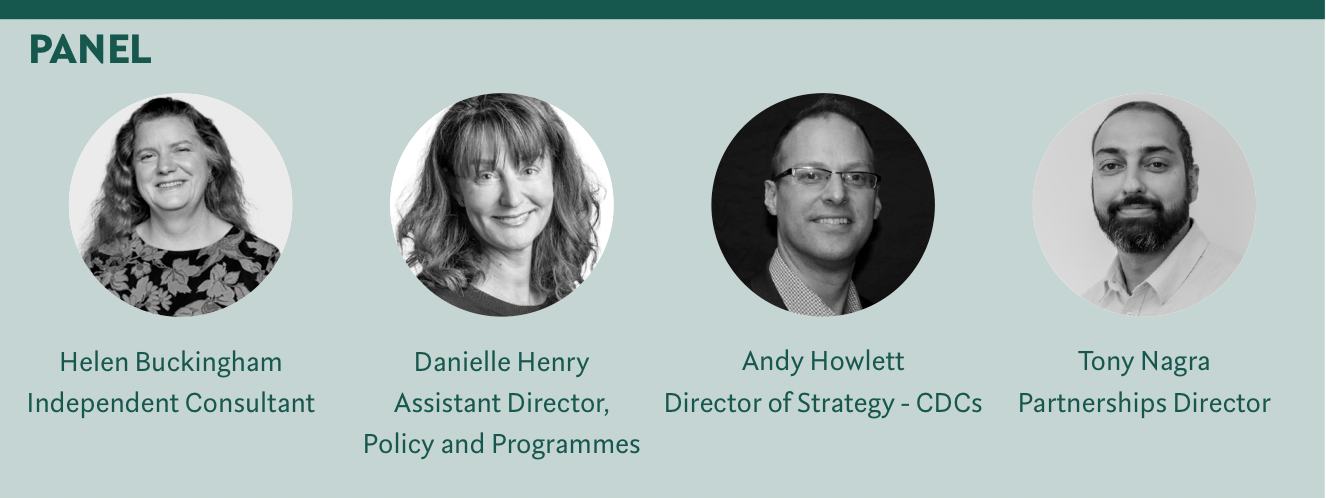
The panel, put together by Darwin Group, includes some of the top in their field. Andy Howlett, Helen Buckingham, Danielle Henry, and Tony Nagra all came together to have this tightrope discussion to try and determine what the independent sector can do to actually help the NHS.
What is the “gap”?
One of the main focuses of the panel’s discussion is the “gap”. What do they mean by this though?
Filling “gaps” in the NHS means finding the places where NHS is struggling to maintain services. These are often areas that the independent sector can and does support.
“We should focus on high-volume low-complexity work,” Howlett says.
The panel seems in agreement that this is the kind of work that the independent sector can provide a good value. Between them, they discuss the common forms; day case clinics, rehabilitation, “prehabilitation”, and even diagnostics.
Where we struggle is with “short termism”
The panel seems especially interested in rehabilitation, specifically the form that often unnecessarily takes place in an acute hospital setting that is not needed.
“There are a lot of people who would benefit from a stay in an in-patient environment that isn’t an acute level hospital, where at the moment they tend to get stuck. This is not the best place for them and is often very expensive,” Buckingham explains.
She also infers that these stays can also be unnecessarily long. “We are also looking for efforts in “prehabilitation” that can reduce [a patient’s] length of stay.”
Between reducing the acuity of the stay, and reducing the length, the price of the total treatment pathway can be significantly reduced.
If we can prepare, we can provide a great service for the public
This can be impactful to the healthcare system as a whole when you consider the number of elderly patients that could be stepped down from a hospital setting to a community setting.
“Community settings could be GP, leisure centres, or even people’s own homes,” Henry says.
“Patients have a good experience in these locations in high street or retail park locations,” Howlett enthuses. “Their experience is a different planet from an acute hospital diagnostic service. The atmosphere is calm the environment is modern and not medicalised, as well as ample free parking.”
“Diagnostic services often take less than an hour, so you can blend in a visit to the shops, meaning it becomes simple, easy, and less stressful,” Howlett adds.
A high street optometrist can refer directly into the independent sector via ERS
In fact, the panel seems to think that patients can be stepped down further even from a community setting if the situation allows. “I think it is worth thinking about people being treated at home,” Henry says. “We keep hearing that care at home is the direction of travel for the NHS, and now we’ve got virtual wards being delivered by the NHS.”
If options are provided to care for these less acute patients more economically, especially in the high volumes there are, then this could reduce costs all around.
Do what you do best
“Specialism leads to efficiency,” says Henry.
Most of the panel disagree with the term “cherry picking” for the activities of the independent sector. They express that this is a misinterpretation of the reasoning behind the sector’s selection of services.
The independent sector does what it specialises in, and does it well. Doing high-volume, low-complexity work, like cataract surgery as Henry examples, means the staff and business can use their familiarity and focused daily operations to create efficiencies.
Huge technology might be the size of a matchbox [in ten years], we just don’t know
But in order to create this familiarity, and therefore efficiency, the companies must have a reasonable expectation that activity flow will be consistent. “Where there is a reasonable expectation that activity will flow, the independent sector can take on the risk of that volume,” says Howlett. "We do that all the time at InHealth. Where we struggle is with “short termism”.”
What Howlett means by short termism, is a Trust asking for 50 cases to be performed one day because they are overloaded, but then none for weeks. This is not going to create efficiencies and will not create two sided value to the independent and public sectors.
Nagra echos Howlett’s concerns about short termism and goes on to say that independent healthcare leaders will have some big challenges coming up in the future to decide what areas to focus their services on, as well as carrying out this plan.
“If we can prepare, we can provide a great service for the public,” Nagra says.
The financing model
Even if the correct services are chosen to provide for, there are other aspects that the panel thinks it is important to examine in order to get a full picture of how the independent sector can work with the NHS.
“I think there are some really interesting opportunities here for filling gaps where the NHS is experiencing real pressures in services that have relatively low barriers to entry in terms of the investment required,” Buckingham says.
She specifically talks about the need to make the involvement of the independent sector attractive to both itself and the NHS.
It is not only the financing model that needs to be finessed in order to create value and efficiencies to both sectors
The fundamentals behind this is the financing model that underpins any collaboration. “All my career in the sector, we have been saying we must forge strategic relationships, but we struggle to achieve that.”
The reason behind this is the exact “short termism” that Nagra and Howlett discussed.
The risk to the NHS of these last-minute cooperations as opposed to long-term well-planned ones is that you see the relatively cheaper work going to the independent sector and the more expensive work going to the NHS, but average pricing throughout. “That doesn’t benefit anybody,” Buckingham resigns.
The referral system
It is not only the financing model that needs to be finessed in order to create value and efficiencies to both sectors.
One of the major high-volume low-complexity services that the independent sector can provide is diagnostics. And for this to work cohesively, the referral system needs to work smoothly.
I won’t talk politics, but politics will play a part in all of this
Henry explains that a good referral system is one of the reasons that ophthalmology’s wait times are significantly above the national average. “The independent sector has been doing a huge amount for the NHS in ophthalmology. The key reason for this is that a high street optometrist can refer directly into the independent sector via ERS,” Henry says. “This is why activity is up 15% compared to 2019 and wait time is down weeks.”
Part of the referral system working well and letting independent diagnostics fit seamlessly into a wider NHS treatment journey is the digital systems that support this.
“Digital integration between the diagnostic provider and the wider NHS system is fundamental,” Howlett stresses. “This is a major part of any contract we (InHealth) enter into with an NHS partner. Without this integration, a lot of the value from the independent sector is lost.”
The role of estates in this independent NHS balance
When looking at the differences between NHS estates and independent estates, there is a lot to discuss.
The panel agrees that, in general, the independent estates are far more flexible. “A lot of the NHS’s focus on its current existing estates is because of treasury conditions,” Howlett says. “This is hamstringing the NHS.”
Howlett explains that this “hamstringing" tends to be focused on land that is already owned, but the buildings on this tend to be in very poor condition with outdated infrastructure, so there are huge costs to get them to a modern standard. “Whereas, the independent sector is much more agile,” he says.
Henry thinks that the independent sector is not as tied to its existing estate, and is more likely to look to new land to build what they need, which means it can purpose built and economical. Making it more agile in planning.
Community settings could be GP, leisure centres, or even people’s own homes
Nagra explains this agility within the independent sector with an example: “If we have an existing building, and we are using half of it for consolation rooms, could that area be used for complex uses, and could we move the consolation rooms to a temporary or permanent building external to the existing estate.”
Flexibility is one priority, but it fits in with another, future-proofing. Buckingham explains that this should be emphasised as we don’t know what the estate will need in ten years’ time. “Huge technology might be the size of a matchbox, we just don’t know,” she jokes.
Sustainability’s part in this can play both sides. Whilst reusing old buildings can seem like the more sustainable option, the panel discusses that when you dig down into it, this can be misleading. “Fitting out an old building brings sustainability challenges,” Henry suggests.
With the 2024 UK general election happening, this could be a time for great change in the sector
This can be the case as The experts talk about the impact of inefficient energy usage, and lack of suitability when retrofitting as ways that the old buildings will require more than they are worth to remain as healthcare buildings.
Howlett brings up the statistic that over 2,000 NHS buildings are older than the NHS itself. “The existing estate is often not fit for purpose,” he says. “A mindset shift is needed.”
2024 and beyond
With the 2024 UK general election happening, this could be a time for great change in the sector. Nagra knows this will play a part in the immediate future and beyond: “I won’t talk politics, but politics will play a part in all of this.”
The panel agree, the estates in the NHS and the independent sector need to work together if the UK’s healthcare system is going to work efficiently and reduce the grossly long waiting lists. Experts have their plans, but only time will tell how these plans play out.
