Since the outbreak of Coronavirus, and the subsequent response by healthcare operators across the country and internationally, one thing that has become evident is that many hospitals lack the capacity and flexibility to meet the needs of both patients with the virus and those in need of regular medical treatment.
And, with a second wave now a very-real prospect, the UK network of Nightingale and field hospitals is poised to begin taking new patients.
But, in the longer-term could hospital design be improved to make our healthcare facilities more prepared for both mass-scale pandemics and other emergency scenarios, such as natural disasters or terrorist attacks?
We need to be able to divide hospitals into contained areas and use both architecture and M&E design to enable that divide
This is an idea being researched by HKS Architects as part of a wider study into long-term flexibility in healthcare design, which has developed the FleXX Hospital: Surge Scenario model exploring the optimum design of a hospital for pandemic preparedness.
The report has been compiled using real-world findings from the current pandemic and is based on learnings from the rapid adaptations that have been made to facilities in the UK and US since the spring.
A primary focus of the FleXX Hospital: Surge Scenario concept is to create adaptable facilities that enable day-to-day operations to continue alongside a pandemic – or other emergency scenario – something that many healthcare facilities around the world have struggled with in the face of this outbreak.
The design has pandemic preparedness built in from the outset and challenges the notion that hospitals are fixed and static buildings, instead designing them to be both flexible and adaptable.
And, with many general hospitals taking more than a decade to build from initial concept to opening, this approach will also address the problems associated with rapid changes to service delivery and the evolution of technology which often mean that buildings are unfit for purpose by the time they are completed.

Sophie Crocker
Speaking to BBH, Sophie Crocker, an architect and health researcher at HKS Architects, explains: “In recent months we have not just been seeing the short-term impact of Coronavirus, but the long-term impact that is having on routine healthcare.
“In many hospitals levels of elective care have been running at 15-20% of normal, suggesting a backlog will be in the millions.
“Through our FleXX concept we are looking at how facilities can continue to offer both COVID-related and other routine and emergency care, and that’s to do with being able to accommodate a surge in capacity and being able to isolate that surge.
“We need to be able to divide hospitals into contained areas and use both architecture and M&E design to enable that divide.
This year has shown us that we can’t continue to look at flexibility and design in terms of years, but we must look at it in terms of a day, or a month, or an hour
“If we are prepared for this then everything can kick in sooner.”
HKS principal and design director, Dan Flower, adds: “To carry out this research we got together with US and Middle East teams and healthcare providers to really question what we are doing now and asking ‘is that fit for the future, or is there a new way to think about things?’.
“When we think about designing hospitals are we planning for the great event?
“A lot of our study is asking ‘are we starting off by asking the right questions when we draw up briefs for new hospitals and how can we change that to enable greater flexibility’.
“The FleXX model enables a facility to be future ready; to respond to changes in medical processes and technology, shifting demands, and increasing use of developments like telemedicine and remote consultations over 5-10 and 20-plus year periods.
“The aim is to ensure a hospital can continue to perform effectively for its full lifespan and, as medical needs shift, to provide alternate programmes such as additional R&D space and patient hotels.”
The model works on five major principles - Versatility, Modifiability, Convertibility, Scalability, and Flow – of air, resource and people.
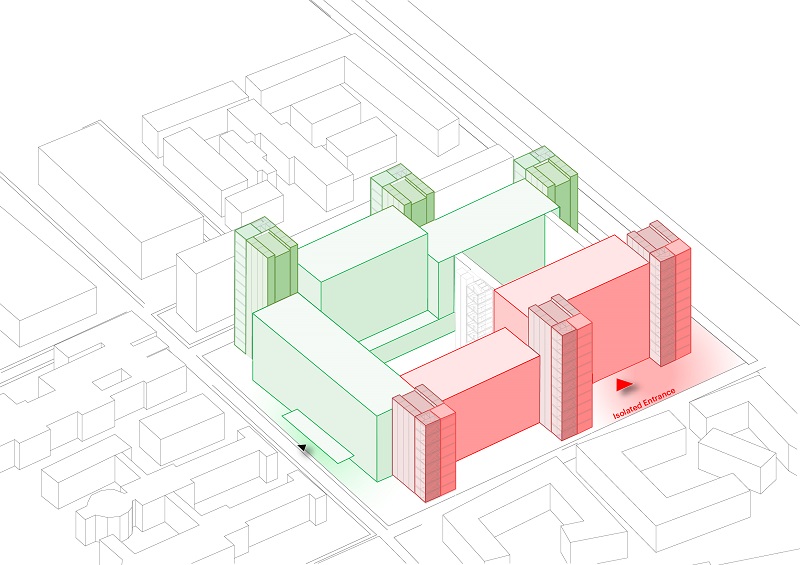
At the peak of the pandemic, the infected zone bed count can reach two thirds of the total number of beds in the facility with double occupancy, while retaining two thirds of the beds for regular operation. Function and circulation are completely separated
And key to delivering these are adhering to a ‘regular grid’; putting service and vertical circulation cores to the perimeter of the building; and standardising high-intensity and low-intensity MEP requirements for slab-to-slab heights. This approach means the interior of buildings can be much more effectively planned at departmental and room-by-room level, and can change function relatively easily.
The Midland Metropolitan Hospital, designed by HKS, is currently on site and uses this ‘regular grid’ approach.
“Following this approach means that, as changes are needed in the design it is not too difficult to make these,” said Flower.
“By moving things like ventilation to the outside of the building you are not constrained as any new risers, for example, are not going into the main building footprint.”
Coronavirus has made us ask will we be able to look back and say that, as a generation of designers, and the wider healthcare community, we responded effectively and did we leave the estate in a better way than we found it?
The Surge Scenario report introduces the principles of pandemic preparedness; protecting the threshold, separation of flows, and signposting risk and required behaviours.
Crocker said: “Flexibility is really important to factor into design moving forward.
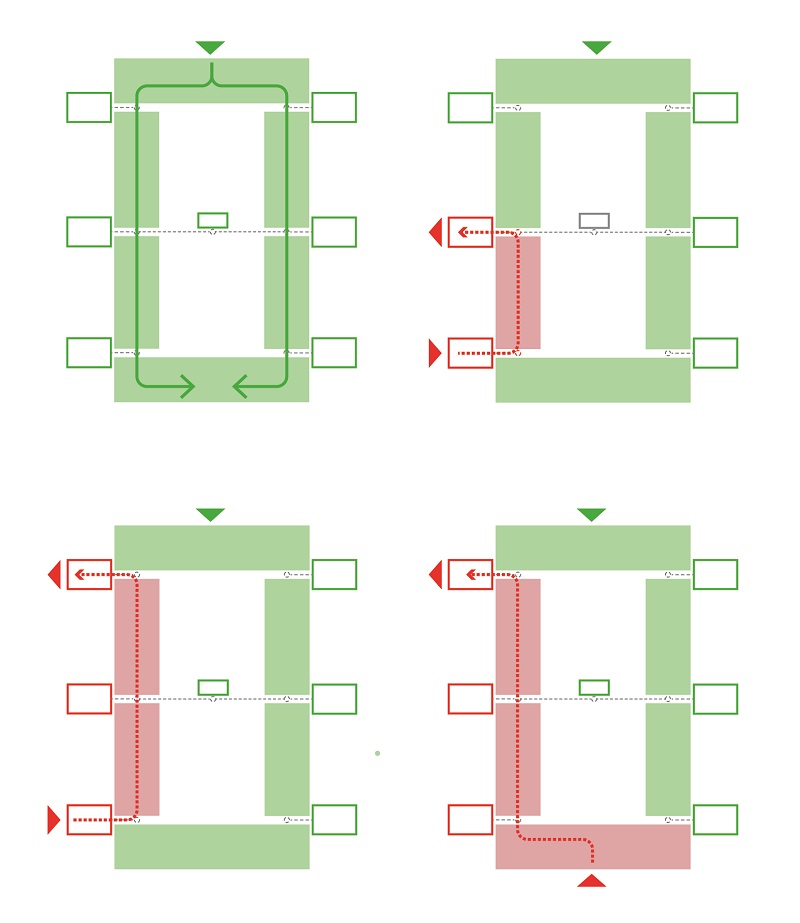
Separation of flows is a key principle of pandemic preparedness. Separating the flows of people, ventilation and resources is key for infection control and maintaining regular operations
“This year has shown us that we can’t continue to look at flexibility and design in terms of years, but we must look at it in terms of a day, or a month, or an hour.

Dan Flower
“When we write about or present these principles, it’s not an overarching strategy, but a toolkit of principles.”
The work is part of an extended research project looking at the business case for long-term flexible design. The team is now looking at the return on investment of the various principles outlined in the report to demonstrate their return on investment for short and long-term adaptability needs.Crocker said: “This is not a finished project and conversations with estates managers would be very welcome to keep the feedback loop going.”
Flower adds: “The Government has signalled its intent to renew the healthcare estate and, while there is no one-size-fits-all approach and no two hospitals are the same, we have tried to test some ideals and look at how they support this idea of adaptable functionality.
It is really important we change the way we do things or it is going to be the same knee-jerk responses every time
“Coronavirus has made us ask will we be able to look back and say that, as a generation of designers, and the wider healthcare community, we responded effectively and did we leave the estate in a better way than we found it? And did we make adjustments that were reasonable and appropriate?
Crocker concludes: “It’s all about planning for change.
“People think we build infrastructure and once the buildings are done, they are done. But we are trying to demonstrate that’s not necessarily the case and it does not have to be, and shouldn’t be, for healthcare buildings.
“It is really important we change the way we do things or it is going to be the same knee-jerk responses every time.”
