Q: The pandemic has prevented many patients from seeking in-person services, particularly those suffering from heart attacks or strokes. What has been the knock-on impact for cardiologists?
A: In the initial stages of the pandemic we were seeing patients presenting late with stroke and heart attacks, often with devastating consequences.
Patients suffering heart attacks were attending hospital several days – or in some cases, weeks – after the initial event, sometimes with significant irreversible heart damage causing heart failure.
Similarly, patients who are suffering with strokes who do not present early to hospital – usually within a few hours – have more significant long-standing symptoms.
Patients need to understand that, while COVID-19 is a dangerous virus, there are consequences of missing out on effective treatments.
Both heart attacks and strokes are time-crucial events, which can usually be treated well if caught early.
The golden-hour rule still applies: those who get urgent and appropriate treatment can often dodge the most-important complications, including long-term damage to the heart and brain.
COVID, or no COVID, symptoms of a heart attack or stroke are a medical emergency and should warrant urgent admission to a heart attack or stroke centre via ambulance.
Q: What were the biggest challenges you faced when pivoting your approach to providing care to patients during the pandemic? And how did you overcome them?
A: The biggest challenge when providing care during the pandemic was being able to continue to offer a safe, COVID-secure service within the rapidly-changing environment.
Guidance and regulations with respect to provision of safe working and consulting measures for staff and patients were constantly shifting.
However, one of the best outcomes has been the strong cohesion seen among all teams across the hospital, but particularly within cardiology.
Strong leadership has allowed us to influence decision-making at board level of the hospital trust, helping us make rapid moves to stay ahead of the COVID-curve.
Q: What are the benefits of introducing a greater number, and variety, of digital technologies into cardiology, both for patients and practitioners?
A: The health crisis has brought into sharp focus the need for more-modern and innovative ways of working.
Part of the post-COVID ‘new normal’ will involve the introduction of novel digital technologies, including devices which can be delivered directly to the patient’s home.
For example, one of the most-common referral reasons in cardiology is heart palpitations. And digital technologies can be very helpful in allowing the documentation of heart rhythm abnormalities (arrhythmias) during a patient’s symptomatic episodes.
If a patient has short-lived, intermittent arrhythmias, or if a full disclosure of heart rhythm is required for longer continuous periods, patch-based devices are extremely useful.
These are small devices – such as the Zio by iRhythm Technologies – which can be posted directly to the patient, who typically find it very easy to apply.
The adhesive chest patch is then worn for the recommended amount of time – for up to two weeks – which allows every heartbeat to be analysed, and correlated to symptoms.
Once used, the patient can simply post the device back in a self-addressed envelope, with a physician then going on to make a diagnosis based on the recorded data.
In addition to devices that allow for initial diagnosis, hand-held mobile two- or six-lead Electrocardiogram (ECG) devices are now also available in the form of the AliveCor Kardia mobile device, and the Apple Watch Series 4 or higher.
Using these simple devices, patients are able to record typically 30 seconds of an ECG and download the data as a PDF, which can then be shared via email with their physician.
Physicians who have an AliveCor device in clinic may be able to immediately record a patient’s (or relative’s, or friend’s) ECG trace, even in the absence of a formal 12-lead ECG machine, therefore tracking activity over time as a means of ongoing management.
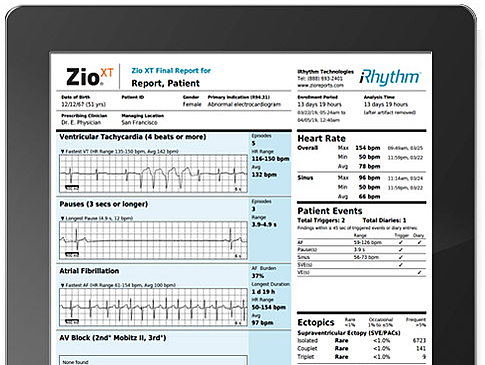
iRhythm Zio could have a major impact on current testing protocols for heart conditions
Q: What can we do to ensure innovation in cardiology continues post-pandemic? And how important is it to the future of healthcare?
A: Innovation in healthcare in crucial, much more so in the ‘new normal’ environment and beyond.
Minimising unnecessary patient contact points – and avoiding exposure for frail and vulnerable populations – are going to be long-standing challenges.
These are hurdles that can only be overcome by innovative individuals, or departments, championing the transition to a new service delivery pattern.
Partnerships that are able to capitalise on, as well as co-create, new technologies with industry and academic institutions will be key.
Only then can we deliver safe, robust, clinically-reliable pathways which will allow healthcare services to adapt rapidly in the face of repeated future challenges, even beyond COVID.
