Outdated and poorly-laid-out healthcare buildings, in dire need of repair and modernisation, are hampering the efforts of doctors to provide safe and quality care to patients, reveals a report from the British Medical Association (BMA).
The report is based on research and analysis by the BMA, including feedback from doctors through an online survey conducted in February 2022.
And it calls on all UK governments, across the four nations, to provide the necessary funding to urgently clear maintenance backlogs – or decide to rebuild sites that may no longer be appropriate to repair – in order to protect doctors and patients, and to prevent the list of remedial repairs required growing further.
Through the BMA survey 38% of doctors reported that the overall physical condition of their workplaces is either ‘poor’ or ‘very poor’, with 43% saying it had a negative impact on patient care.
Also included in the report are a series of first-hand testimonies from doctors revealing worrying safety incidents.
As well as issues around disrepair, including leaking ceilings, peeling walls, and faulty electrics; doctors also commented on how old, cramped, and poorly-designed hospitals and GP practices are incompatible with running a 21st-century health service, with concerns around appropriate ventilation and infection prevention and control (IPC) measures being paramount.
Lack of space often means doctors do not have suitable rest facilities, room to accommodate additional staff, or places where clinicians can discuss sensitive and confidential information with patients and their families.
The backlog maintenance bill for the healthcare estate in England alone is estimated to be around £10.2billion
As well as calling for UK governments to provide the funding to address backlog maintenance, the BMA recommends that doctors should be empowered to immediately raise concerns where building conditions present a risk to patient survey and that all UK governments must launch transparent and independently-audited national reviews of the condition of the primary and secondary healthcare estates, including an urgent review of IPC and ventilation, with dedicated funding provided for improvements and retrofitting.
“It is a national scandal that a continued failure to invest properly in the bricks and mortar of our hospitals and GP practices is threatening safe patient care,” said Dr Latifa Patel, BMA representative body chairman.
“The scenes described by our members in this report are not what we would expect to see in a 21st-century health service in one of the world’s richest countries.
It is a national scandal that a continued failure to invest properly in the bricks and mortar of our hospitals and GP practices is threatening safe patient care
“Yet, for doctors, the shocking accounts of leaking ceilings, peeling walls, and faulty electrics will come as no surprise, as the state of disrepair is so endemic across the NHS.”
A second report, published alongside this one, reveals further frustration from doctors with the digital infrastructure of the NHS, with out-of-date, slow, and incompatible IT systems and hardware costing valuable staff time and again putting patient safety at risk.
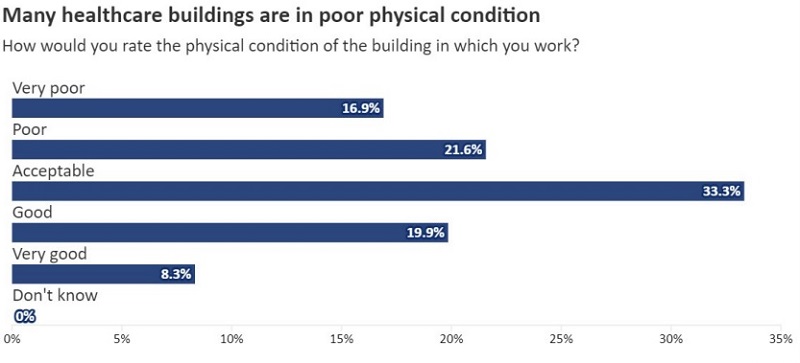
17% of respondents rated their buildings as 'very poor'
Key findings from the report
- Healthcare estates have been starved of capital funding, with long-term underinvestment creating vast maintenance backlogs, preventing vital expansion and modernisation, and undermining the wellbeing and safety of staff and patients
- An alarming 38% of doctors answering the BMA’s 2022 estates and IT survey say the overall physical condition of their workplaces is ‘poor’ or ‘very poor’
- 43% of doctors surveyed said the condition of their workplace has a negative impact on patient care – illustrating the extent of this crisis Crumbling buildings and infrastructure often force wards and beds to close, compounding a wider lack of space across healthcare estates and contributing to ever-expanding waiting lists
- A lack of space for hospitals beds and GP consulting rooms limits access to care for patients and can lead to longer waiting times and care being provided in corridors
- Insufficient space in hospitals and GP practices is hindering doctors’ training and preventing the recruitment of additional staff
- Over two thirds of respondents felt the condition and configuration of their workplaces would not allow for appropriate ventilation and infection prevention control measures in the event of a further wave of COVID-19 or a future pandemic
- Much of the healthcare estate is incapable of supporting badly-needed digital transformation
- Car parking charges at and poor transport options to the UK’s healthcare estate continue to be a lingering issue among doctors, as well as limiting efforts to reduce the carbon footprint of healthcare services
- Estates are the primary contributor to UK health services’ climate impact, with outdated heating systems and inefficient buildings increasing both costs and emissions, but governments and providers are failing to adequately invest in addressing this challenge
- Doctors are inadequately involved in the planning of estate projects, meaning infrastructure plans all too often fail to capture their extensive insight into how healthcare estates do, could, and should serve the needs of frontline staff and patients
For doctors, the shocking accounts of leaking ceilings, peeling walls, and faulty electrics will come as no surprise, as the state of disrepair is so endemic across the NHS
Key recommendations
- Significant increases in capital funding must be provided in order to address long-term underinvestment in healthcare estates
- All UK governments must launch transparent and independently-audited national reviews of the condition of the primary and secondary care healthcare estates, building on existing work where appropriate, assessing the availability and standard of staff break space, the quality of staff training spaces, and the efficacy of infection prevention control and ventilation measures
- All UK governments should provide ringfenced funding to clear existing maintenance backlogs to protect doctors and patients, produce plans for when and how those backlogs will be resolved, and publish full maintenance backlog figures annually
- Every doctor must have access to quiet, comfortable office spaces where they can discuss confidential matters in private
- All providers should ensure break spaces are available for all staff, and that all new buildings and expansions include guaranteed, high-quality break spaces compliant with BMA guidelines
- All UK governments and health services must link their estates and digital transformation programmes and provide necessary funding to ensure that all healthcare environments are capable of supporting new technology, IT systems, and high-speed Wi-Fi
- Capital investment must be provided to create additional beds and clinical space in hospitals and GP practices, through both the safe expansion of existing premises and new builds where needed. This must include affordable funding options for GP premises expansion and improvement, to properly accommodate nationally-mandated recruitment of additional staff
- All healthcare providers and systems must carry out an assessment of transport options available for staff and patients. Healthcare providers must also improve car parking facilities, particularly where alternative transport options are not viable
- Funding should be made available to GP practices and hospitals to improve their accessibility, particularly for people with disabilities and limited mobility
- UK governments must better support healthcare organisations to meet their carbon reduction targets; this must include ringfenced capital funding for improving the sustainability of health service estates across the UK
- All estates planning – including plans for individual hospitals and buildings – should closely involve doctors, staff, and patients
