The UK has one of the world’s most-highly-respected mental health systems.
When Canada inspected the best examples in the world, including Australia and Norway; it was the UK’s Improving Access to Psychological Therapies (IAPT) model the country chose to follow.
For better mental health care in Canada, look to Britain, they said.
And, as an IAPT service provider in the UK; Ieso has seen huge growth in the rollout of our one-to-one mental health service that is delivered via an online platform.
We enable patients to engage with cognitive behavioural therapy (CBT) treatment online through text-based instant messaging over a secure cloud platform.
When Canada inspected the best examples in the world, including Australia and Norway; it was the UK’s Improving Access to Psychological Therapies (IAPT) model the country chose to follow
This is usually done out of hours, which offers convenience to patients and saves over 120,000 journeys to attend face-to-face appointments each year.
Building a picture
Uniquely, it has also allowed us to build a sizeable data bank of over 220,000 hours of real-world therapy transcripts.
This type of data has never been collected at scale before and our unique data set has allowed us to build three primary technical capabilities so far, and is informing a roadmap of digital therapeutics under Ieso’s Eight Billion Minds programme that we hope will see the end of unmet mental health needs globally.
The capabilities to date include patient data record analysis to enable precise and personalised therapist skills improvement; deep learning analysis to find out what elements of therapy are clinically most effective; and human-in-the-loop AI assistance to prompt therapists and support accurate diagnoses.
CBT is typically taught via lectures, clinical skills workshops, and clinical supervision.
Therapists are assessed using a variety of methods including academic writing in the form of essays or case reports, and the submission of self-selected tapes of live therapy sessions.
Despite the extensive array of pedagogical processes; many trainees struggle to bridge the theory-practice gap. In addition, it is hard to assess whether trainees are consistently delivering interventions that demonstrate fidelity to the model.
Once qualified, CBT therapists have very little feedback in relation to their clinical work.
By making treatment tools readily available to all, we can prevent people dropping through the gaps or having to go back to the bottom of the waiting list if their symptoms return
And, while it is standard practice for CBT therapists to provide recordings of their clinical work to their supervisors; it is only done for a handful of sessions each year, and the therapist themselves get to select the sample.
If a patient has a poor experience of CBT they will be reluctant to try that approach again and they effectively become immunised against that treatment modality.
While IAPT has radically improved transparency of clinical outcomes, services still don’t know why some therapists get better outcomes than others.
At Ieso, we use technology to address this challenge.
Samples of individual patient transcripts are routinely reviewed by a therapist’s clinical supervisor, and therapist records are assessed with machine learning to show which therapists are doing well and which need additional training and support to improve patient outcomes.
Improving your chances
We have also integrated artificial intelligence into the Ieso ThinkWell therapist platform as a clinical decision support tool.
It uses an AI model to support the clinicians when deciding on a patient’s primary presenting problem.
This gives them the best chance of making an accurate, evidence-based diagnosis, and enables the delivery of more-effective treatment.
The system also helps therapists identify patients who are likely to drop out of treatment, allowing them to take action to increase chances of engagement and recovery.

Ieso has begun to collect data on what mental health therapies work and how they are best delivered
Ieso’s method of delivering CBT through written conversation means that, unlike spoken sessions, the efficacy of treatments can be measured, improved, and ultimately tailored to the person receiving it.
Deep learning analysis of the historical transcripts has enabled us to complete a scientific study of anonymised recorded therapy transcripts to determine which features are associated with an improvement in patient symptoms.
It is a very-exciting time in the history of technology in mental healthcare and the UK is once again at the forefront of these developments
It would be impossible for humans to analyse such a large data set and the machine analysis provided valuable insights into the relationship between therapy content and clinical outcomes that were previously unknown.
The findings (Figure 1 below) showed that when treatment contained a greater quantity of CBT change methods, patients were more likely to show an improvement in symptoms.
Patients were less likely to improve when sessions had increased quantity of ‘non-therapy’ content (see ‘Other’ in Figure 1).
This information was fed back to therapists through training and is built into the platform AI to improve suggested responses to therapists.
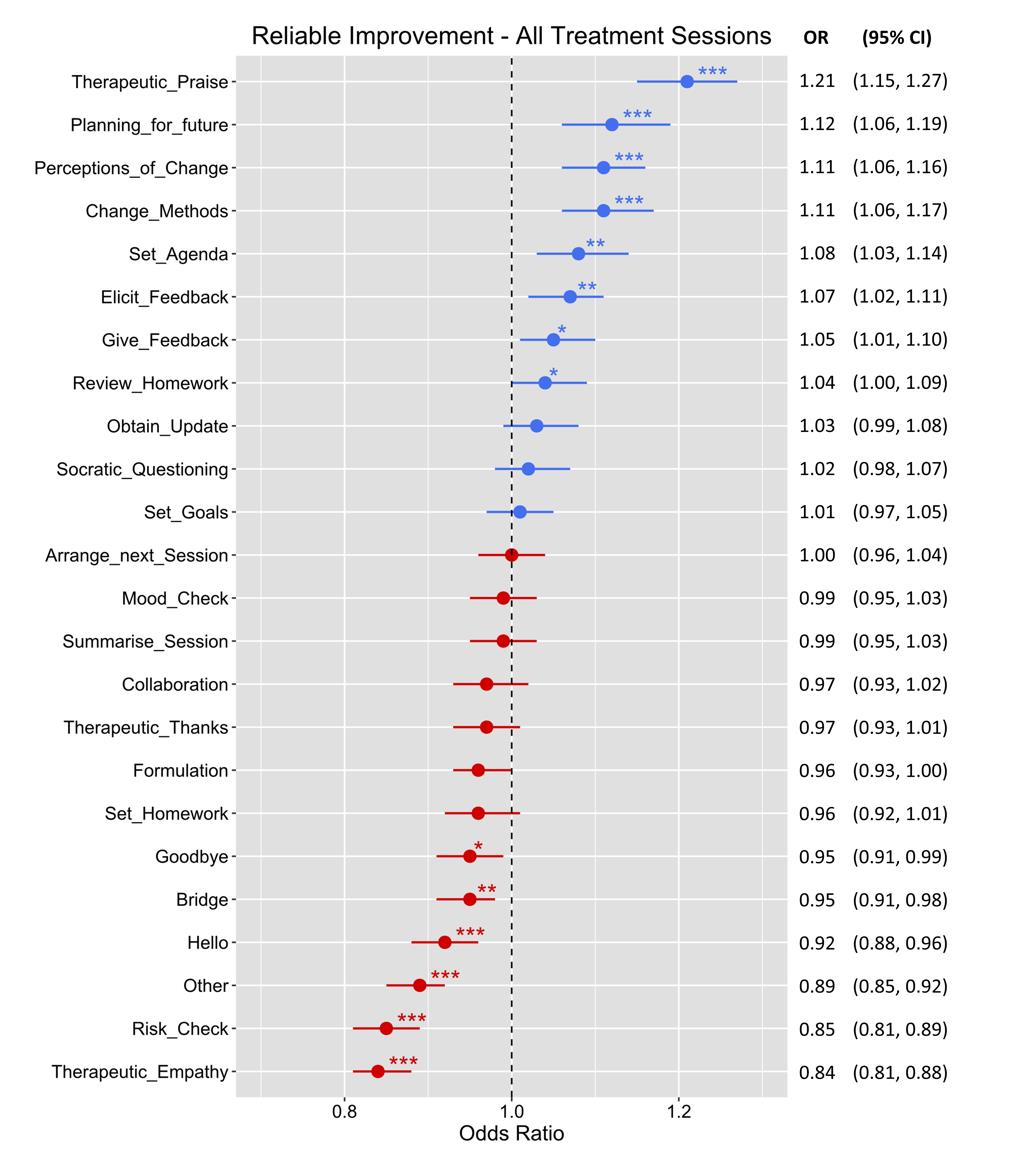
Figure 1: Analysing the content of therapy sessions and correlating different content types with the patient’s chances of improvement. Items in blue indicate higher likelihood of improvement, while items in red correspond to lower likelihoods. The presence and number of asterisks indicate presence and increasing levels of statistical significance
Opening doors
This ability to quantify clinical efficacy of therapy opens the door to many other medical advances such as where there are co-morbidities between mental health and physical disease, for example Ieso’s current trial investigating co-morbid depression with diabetes.
While the digital platform enables us to use deep learning and AI to learn what works, which therapists are performing best, and constantly improve outcomes; the real advances in mental healthcare come when we are able to develop technology using this data to create digital therapeutics.
Figure 2: Utterance sequencing: decoding the ‘chemistry’ of effective psychotherapeutic intervention. Each row is a therapy session with more than 190 utterances tagged by a deep learning model into 24 therapeutically-relevant categories. The tags have each been assigned a colour
The insights come from large-scale analysis of therapy content (Figure 2 above), and from understanding, not just the elements of therapy; but also the structure of sessions, by looking at each therapist utterance in the context where it occurs (Figure 3, below).
This next step in technology, being developed under the Eight Billion Minds programme, will enable us to build and test triage tools, create apps for in-between appointments, and for the alleviation of lower-level severity symptoms.
These can all be tested and validated in a real-world clinical environment to prove both efficacy and effectiveness.
This will be the turning point in mental healthcare as we know it.
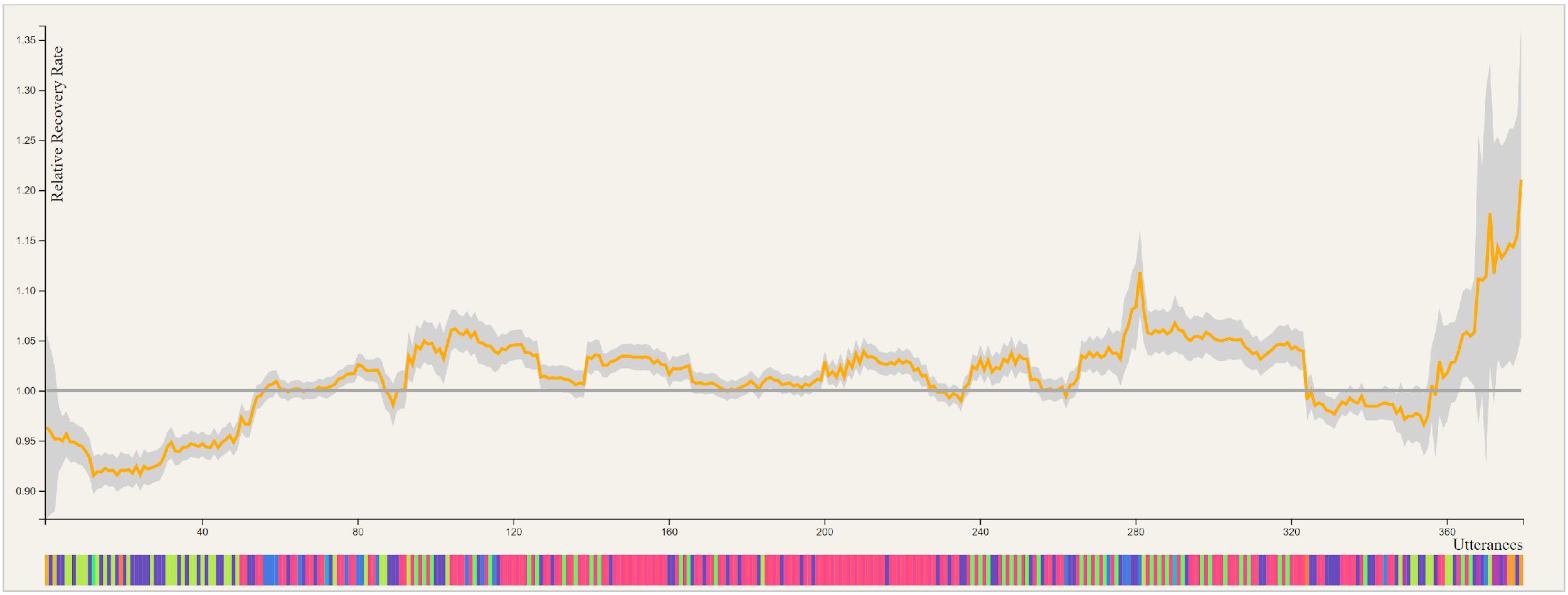
Associating utterance sequences with clinical response to treatment. Sequence of tags aligned against 200,000 hours of therapy using the Smith Waterman Local Alignment algorithm. The graph represents the recovery rate associated with the sequence of utterance classes occurring at each site. For reference, the horizontal line indicates the average recovery rate; areas above the line represent increased chances of recovery for patients whose treatment contains each local sequence
By making treatment tools readily available to all, we can prevent people dropping through the gaps or having to go back to the bottom of the waiting list if their symptoms return.
We will be able to help patients around the world who just can’t access mental health therapies.
It is a very-exciting time in the history of technology in mental healthcare and the UK is once again at the forefront of these developments.
