Health inequality is a growing problem, but is still too often discussed separately from the core business of the NHS.
Patients are treated through siloed care pathways, with conversations about why some populations have poorer health outcomes often treated as an aside.
And the pandemic brought this into greater focus, especially around issues of digital inclusion.
Technology rolled out across the NHS in response to COVID-19 often widened the gap between those who could access online services and those who couldn’t.
The benefits of an ICS
So, what can we do?
I’ve always been passionate about digital inclusion and equitable access and outcomes and when I came into post two years ago, I was excited by the freshness of working for an ICS and the opportunities it created.
We’re a new type of organisation, working as a system across Norfolk and Waveney.
Technology rolled out across the NHS in response to COVID-19 often widened the gap between those who could access online services and those who couldn’t
We work across the public sector, with health and social care, councils, and with voluntary organisations.
What this means is we can tackle health inequality and exclusion in a person-centred way.
The ICS gives us the opportunity to work across organisational boundaries, to test our assumptions about exclusion, and to leverage the work that happens at the level of individual places.
Fixing digital inequalities
At every stage, we’re ensuring that our digital projects fix inequalities.
We’re planning on implementing a pan public sector hub-and-spoke model that provides personalised support to our excluded groups.
Our plan is to gain the wider benefits of digital inclusion by engaging people – not only in health services – but more broadly in society.
If you’re an elderly person, for example, and your GP detects you’re socially isolated, they can refer you to a central digital inclusion service.
From there, you might get passed to a library or voluntary service who can provide connectivity or a device with 5G, plus the ongoing support to use it.
The ICS gives us the opportunity to work across organisational boundaries, to test our assumptions about exclusion, and to leverage the work that happens at the level of individual places
This allows you to order a repeat prescription, but also to food shop online or video call your family, with positive benefits for wider wellbeing and health.
Asking people to go to an appointment at an unfamiliar location can create unnecessary barriers. So our ambition, going forwards, is to work towards using services that people already access to provide a trusted contact point.
If you’re already known to a church group or domestic violence shelter, for example, you might receive support there.
Through our community partnerships, we can build a network of digital tools and skill provision.
If a partially-sighted person, or family member, needs a speech-to-text reader, then we’d like to be in a position to point them to our trusted toolkit.
Once a person has access to our network, they can download tools ahead of health need.
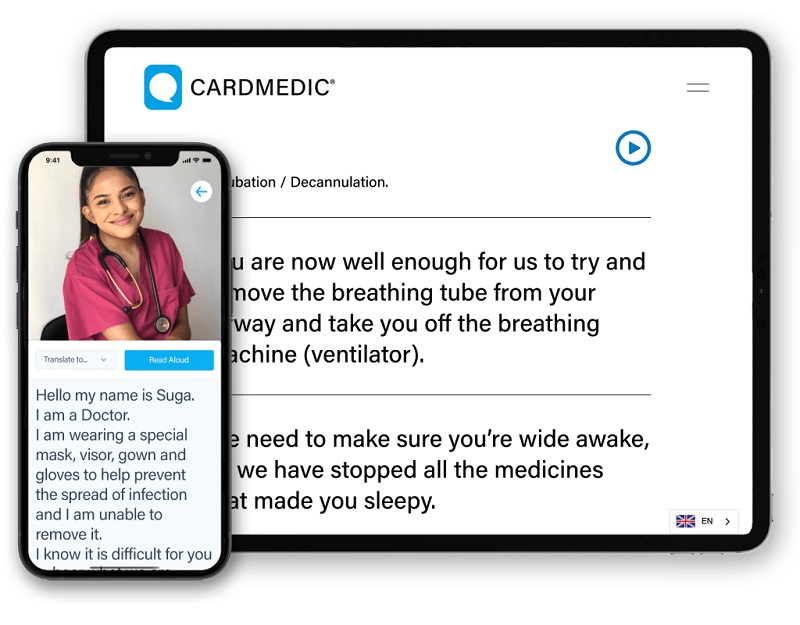
CardMedic is an example of how digital tools can provides instant access to communications options to improve engagement with healthcare professionals
Building an inclusive service
We need to build a future where every service is digitally inclusive.
As the Good Things Foundation Widening Digital Participation report found in March 2020, digital inclusion pays for itself in better mental and physical health, and stronger participation in the economy.
For every pound spent, £6.20 is made back.
With this in mind, I’ve been using my personal learning network to identify new ways to increase inclusivity.
I’ve followed companies, such as ThriveByDesign and CardMedic, an award-winning digital tool that provides instant access to communications options to improve engagement with healthcare professionals.
There’s only so much we can do as a system organisation and on my wish list for the NHS nationally is a better system for picking up on digital innovation
CardMedic is designed to help patients with a language barrier, visual, hearing, or cognitive impairment, or to communicate through PPE. It’s unique in its space and caught my attention immediately.
One of the issues with digital inclusivity tools, though, is that they’re often seen as only affecting excluded communities, but digital inclusivity applies to everyone.
People often struggle to retain emotionally-sensitive medical information, such as a cancer diagnosis.
Tools like CardMedic allow any patient to review the basics of a hospital procedure or consultation – helping them to feel more secure in their care.
Applying innovation
We’ve been lucky to have built a great team and strong relationships at our ICS.
The public sectors and voluntary organisations in our region have pulled together to implement a digital transformation agenda.
And, as we move forwards with the ICS on a statutory footing, we hope to build on that by hiring good people and implementing innovative technology.
But there’s only so much we can do as a system organisation and on my wish list for the NHS nationally is a better system for picking up on digital innovation.
It shouldn’t be up to us to find products, such as CardMedic, via Twitter. Digital inclusivity should be available to all.




